The Chief Medical Officer of Health Report
Earlier this year, the Chief Medical Officer of Health of Ontario, Dr. David Williams, issued a report entitled: Improving the Odds: Championing Health Equity in Ontario. The report focused on health equity in Ontario and made recommendations for action across different sectors and all levels of government to give every Ontarian an increased opportunity to be as healthy as possible.
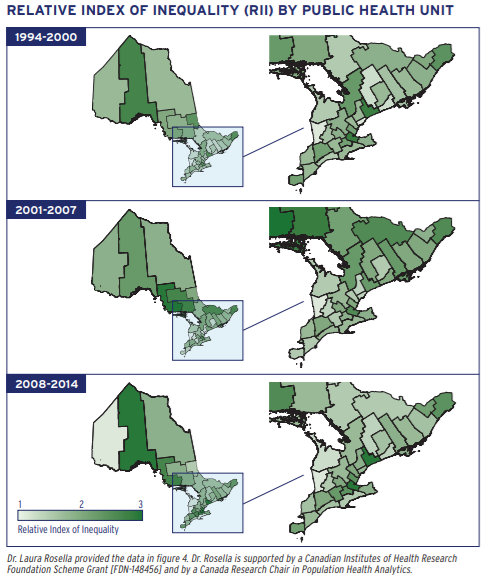
Population Health Analytics’ OPTIMISE project, lead by Dr. Laura Rosella, supplied crucial data for the report to help answer questions about who our health system is and isn’t reaching. The primary usefulness of OPTIMISE’s contribution came from the way it links population data files, socioeconomic status (SES), health administrative data, and vital statistics data.
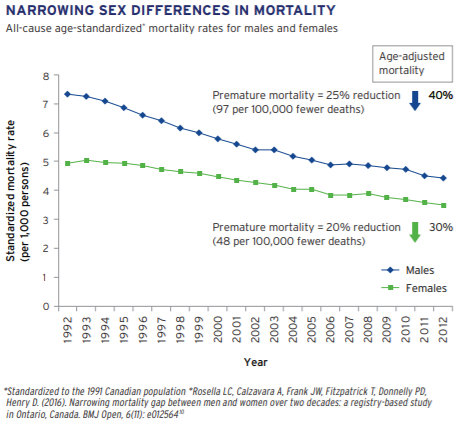
Also included were OPTIMISE’s findings that, in general, Ontarians live longer now than two decades ago, and that the mortality rates in Ontario, as well as the gap in life expectancy between women and men, have diminished.
Initiatives and Outcomes
The report also detailed how “community initiatives supporting social cohesion are key to improving health outcomes”, and that the public health sector was best positioned to do things like: (i) identify the emergence of health inequalities, and generate sustainable interventions; (ii) unite “system-wide and cross-government” bodies to tackle complex health equity issues; (iii) disseminate health inequity data to inform community development efforts.
The ideal outcomes of a strategic investment in health equity research, partnerships and data cultivation (which essentially comprise a new mode by which to approaching health inequity) are: better individual health outcomes, healthier communities, and a lowering of health care and social costs.
A Robust Approach to Complex Problems
As it stood in Ontario in 2016, the top five percent of service users account for 55% of health care spending. The health of all individuals—but also crucially these top five percent of users—relies on a range of factors, including genetics, lifestyle choices, and an array of social determinants such as income, education, access to health services, and social and physical environments (all of which relate to one another on various geographic and socioeconomic levels).
The way to address health inequalities, then, lies not in resisting the complexity of their causes, nor in hunting down innumerable unexplored paths for each tangled origin while the problem continues, but rather in embracing and continuing on with successful methods, like those used by Peterborough (as detailed in the report) to ameliorate their food insecurity issue.
This connecting up of local initiatives with broader system-wide changes to sustainability—from research, to data sharing, to policy making—points the way to a reduction of health outcome gaps.
__________