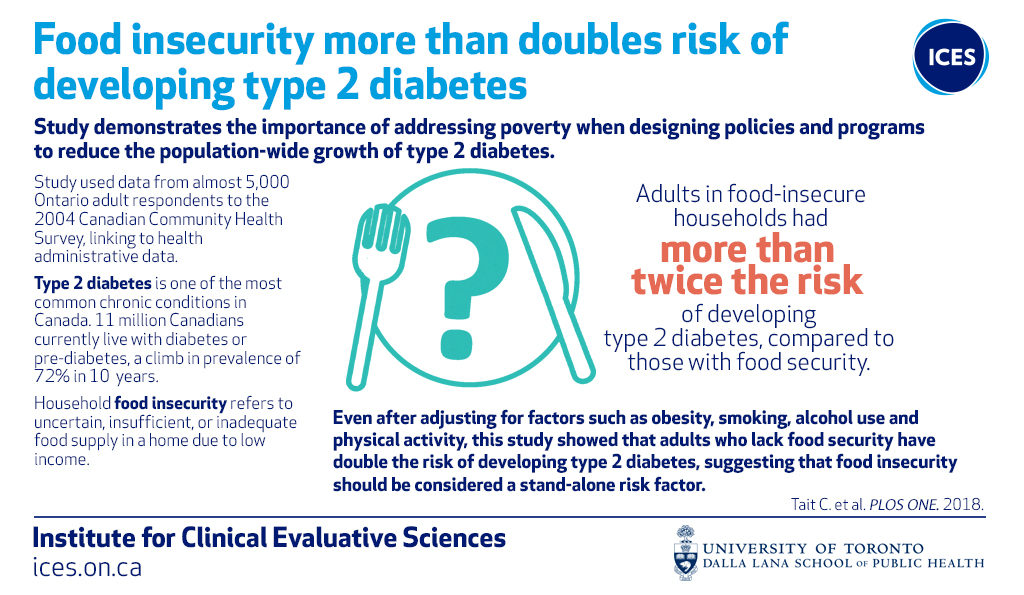
In his new paper, anchored in a population-based cohort study, our Pop Health Analytics team member Christopher Tait, alongside Drs. Mary L’Abbé, Peter Smith, and Laura Rosella, analyzed the association between food insecurity and incident type 2 diabetes in Canada.
 The Role of Food Insecurity
The Role of Food Insecurity
The current landscape of literature surrounding type 2 diabetes largely focuses on lifestyle and behavioural risk factors as targets for intervention, but less attention is directed at understanding the role of upstream social factors that influence type 2 diabetes risk. One such factor is food insecurity, a state of being without reliable access to a sufficient quantity of affordable nutritious food, which has gradually increased among Canadians and been identified as a significant social problem.
Cross-sectional studies have established a link between food insecurity and known diabetes risk factors, and even diabetes itself, but few have assessed the strength of the relationship between food insecurity and incident type 2 diabetes (and never prospectively using a population-based sample). Due to the nature of cross-sectional studies, however, researchers are often unable to determine the direction of the associations found therein (thus valid arguments have been put forth in the literature for both a causal and a reverse-causal association between food insecurity and incident type 2 diabetes). This study suggests a discernable direction of influence.
Grounded Inference
With the directional difficulties mentioned above in mind, researchers estimated the future risk of type 2 diabetes as a function of food insecurity over 12 years of follow up, in a population-based sample of Ontario adults. Their data pool consisted of linked survey (Canadian Community Health Survey) and health administrative data (Ontario Diabetes Database) from The Institute for Clinical Evaluative Sciences. This study marks the premier evaluation of this association in a Canadian context.
The Findings
This study found that those in food insecure households had 2.40 times the risk of incident type 2 diabetes compared to those in food secure households. These results remained robust even after adjustment for several potential confounders and quantitative bias analyses.
Though previous cross-sectional studies indicated that the magnitude of food insecurity and type 2 diabetes association may differ between men and women, there was no meaningful difference in the association according to sex. Men showed a 2.74 times increased risk in type 2 diabetes when food was insecure vs. secure, and women showed a 2.18 times increased risk for the same comparison.
Implications of this Unique Look at Type 2 Diabetes
This study, which is the first to estimate the food security-type 2 diabetes association in a longitudinal population-based cohort study, implies many things.
First, that the association in question may be explained by binge-fast cycles (that is, episodic underconsumption followed by periods of overconsumption—as determined by the cyclical nature of an individual’s social assistance, paycheques, and competing financial needs). These cycles are associated with food insecurity and predictive of insulin resistance in a distinctly different way than by which food insecurity predicts obesity and weight gain.
Second, the results of this study empirically challenge the reverse-causation hypothesis that prior cross-sectional studies could not definitively debunk (an example of this would be the assertion that food insecurity is perhaps not a predictor of diabetes, but rather that once diagnosed with diabetes, individuals are more prone to food insecurity).
Lastly, the findings here firmly establish food insecurity as an independent predictor of type 2 diabetes and reaffirm the need for continued monitoring of the long-term health risks associated with food insecurity.
This study not only demonstrates the utility of linked data when studying the determinants of population-level morbidity, but also highlights a key benefit of upstream monitoring. Continued analysis of individuals’ inability to securely nourish themselves opens the door to possible upstream interventions for type 2 diabetes, and greater future wellness for Canadians who, in their food insecurity, harbour an increased risk of type 2 diabetes.
To read the full study, click here.
